
Mary - PROGRESSIVE GOAL ATTAINMENT PROGRAM (PGAP)
When we started working with Mary, she was a 36-year-old married lady with three school-aged children. She had been involved in a work accident 10 months prior and had suffered an injury to her shoulder. She had maintained contact with her employer during that time but had not made any attempt to return to work. She presented with significant symptoms of depression, was often teary and struggled to get through her daily responsibilities with her family.
When we met, Mary’s main reported issues were her high levels of pain and her overall feeling of being completely overwhelmed by everything she needed to fit into her week. Initial discussions regarding a return to work sent Mary into quite a panicked state, and she struggled to even discuss or contemplate this. Although she was not at work, she was participating in a range of treatments for her shoulder including physiotherapy 3 times per week, massage once a week and GP visits once a fortnight. Mary was extremely stressed about how she could fit all these appointments in as well as care for her family. She no longer felt that she was in control of her own life. She reported that her personal and social life had suffered – she was not meeting with friends, spending time with her husband and felt that she was no longer an active participant in her children’s lives. Mary explained that her behaviour had changed significantly, and reported herself as being far more snappy and critical than usual.
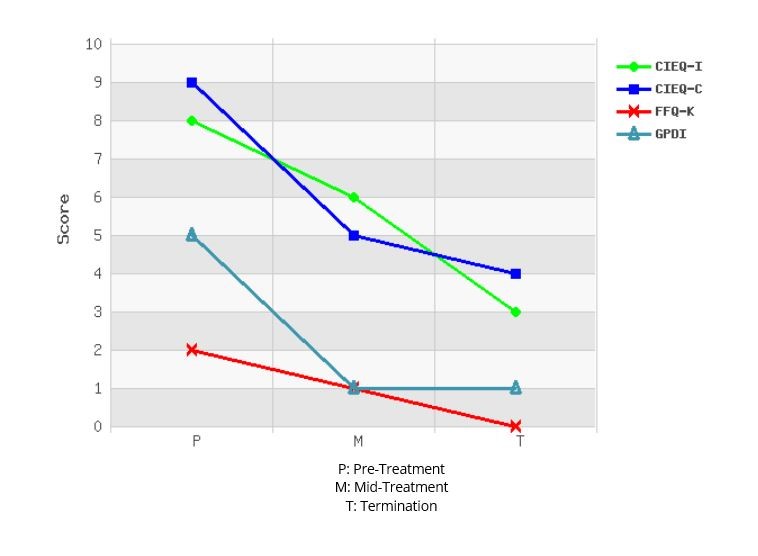
Mary’s initial assessment measures indicated severe reported pain levels, moderate depressive symptoms, severe symptoms of post-traumatic stress and severe levels of fatigue. Her psychosocial measures demonstrated high levels of catastrophic thinking and perceived injustice and moderate levels of perceived disability.
Throughout the 10 week program, we focused on:
- A daily walking program;
- Increasing meaningful activity involvement;
- Planning and scheduling daily activities;
- Focusing on one day at a time so as to not become overwhelmed;
- Goal setting;
- Breaking goals down into achievable parts;
- Addressing and challenging thought patterns relating to her perceived injustice and catastrophic thinking.
Initially, we assisted Mary to focus on the things that were most important to her – her children, husband, extended family and friends. We also did some goal-setting around taking time out for herself. Setting some goals around these crucial elements of her life and then scheduling time to actively engage in meaningful and enjoyable activities gave her a very quick sense of success, achievement and she reported starting to feel some control over her life. The daily walking program assisted in re-establishing a ‘normal’ morning routine where she would get up earlier, shower, get dressed and have breakfast before leaving the house for a walk. She also included her family inthis walk whenever possible, which became an enjoyable time to spend some time together outdoors and discuss their plans for the day which also providing some exercise and fresh air.
By week 4, Mary was ready to start a graduated return to work program, starting on light duties and with reduced hours. Organising a case conference with Mary, her doctor and her physiotherapist really reinforced the importance of giving work a try and gave Mary the confidence she needed to know that everyone was assisting her and monitoring her progress and that if something went wrong she had people to assist her get back on track.
By the end of the 10 week program, Mary was successfully maintaining 3 days per week at 5 hours per shift. She was meeting with friends once per week and had broadened her friendship circle though her school network. She reported feeling more confident as a mother and felt that she had gained important parenting strategies along the way that assisted her to cope. Her assessment measures also noted significant progress with only mild reported pain levels (even though her activity levels had significantly increased), sub-clinical symptoms of depression, mild symptoms of post-traumatic stress and moderate levels of fatigue. Her perception of disability had reduced to low and her perceptions of injustice and catastrophic thinking patterns had reduced to moderate (see graph). Mary had enjoyed the daily planning structure so much that she had made this into an ongoing routine, even on completion of the program. At the end of the program we revised tools and strategies for coping and getting back on track if things started getting difficult again.
Six months on, and Mary has continued and maintained her journey of progress. She is maintaining her pre-injury work hours (4 full days per week) and reports thatshe is enjoying work again. She has continued to use her daily planning structure to not overwhelm herself with planned activities and ensure that she makes time for herself, her family and some social outings. Although she still feels some discomfort in her shoulder at times, and feels that she gets tired more easily than she used to, she is not reporting any pain.
Mary’s case study demonstrates the importance of:
- Focusing on the whole person, including what is happening physically,cognitively, socially, emotionally, relationship-wise and work-wise;
- Involving other key treatment providers in the program so everyone is working towards the same goals;
- Starting goal setting with meaningful life goals if the return to work goals are too overwhelming at that stage;
- Using the success of the life/social goals and activity scheduling towork towards the return to work goals;
- Using very gradual increments and pacing to break large goals down into smaller achievable ones.

