
Recently I read the first “self-improvement” book that has genuinely led to me changing my habits. Atomic Habits by James Clear provides a very simple and practical way to develop good habits (or unlearn bad habits) that can snowball into great achievements and lifestyle changes. He clearly demonstrates how many great achievers get there through the compounding of tiny changes. After the first chapter I noticed the same transient excitement that I often get when I read any “self-improvement” book, but then Atomic Habits introduces a simple and practical model to take that excitement and start making tiny changes after only the second chapter. The one aspect from the introductory chapter that particularly resonated with me was the concept that for a habit to stick it must be in line with our perceived or intended “identity”. An example given is that “the goal is not to read a book, the goal is to become a reader”. If you take on this identity of being a reader then the motivations become much more intrinsic, you naturally ask yourself “is this what a reader would do?”
I will attempt to summarise Clear’s model, but I whole-heartedly recommend reading the book to get the full effect.
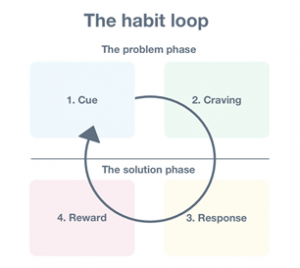
The whole model is based around four stages the mind and body go through when a habit is being developed (usually an entirely unconscious process).
Stage 1: Cue – a piece of information that reminds you of a potential reward (eg. you see your fridge)
Stage 2: Craving – the mind/body motivation for the reward (eg. you get excited by the thought of food)
Stage 3: Response – the action/habit (eg. looking in the fridge and grabbing a snack)
Stage 4: Reward – satisfying the craving (eg. eating the snack)
Here is how the model uses these four stages for intentional habit-building, and how I started to apply each element to help me do exercise after work rather than flopping on the couch and struggling to get the motivation to get back off the couch. The model also works in the opposite way to unlearn bad habits.
Overall identity: a fit and disciplined person
Stage 1 (cue): Make the cue for your intended habit obvious (I used Clear’s “habit stacking” method by identifying a habit I already have – taking off my work shoes – to be the cue for putting on my activewear; an obvious cue for exercising).
Stage 2 (craving): Make the intended habit attractive (Clear explains how our bodies crave an immediate response, so thinking about the final goal such as running a marathon will not elicit an internal craving for the habit. For my exercise habit I am using Clear’s example of thinking about the immediate after-effects of exercising, thereby developing a craving for the exercise-high).
Stage 3 (response): Make the intended habit easy (I am only committing to 5 minutes of walking/running/yoga and even if I stop then, it will still contribute to the repetition required to solidify the habit – as you could guess I have always continued after 5 minutes since the hard work of getting going is already done).
Stage 4 (reward): Make the intended habit satisfying (I take a moment to revel in the exercise high, allow myself the slow walk cool down, feeling high and mighty, and grant myself the guilt-free evening on the couch).
Some of the elements may seem like common sense but often we miss one part, and it is the one thing that leads to a failure to keep up with new habits. I encourage you to try applying the model to a habit you would like to develop and see if there is something missing. Happy habit-forming!

This research project sought to provide Australian research on the Progressive Goal Attainment Program (PGAP). The PGAP aims to reduce the impact of four psychosocial risk factors known to be associated with work related disability. The psychosocial risk factors included are perceptions of injustice, catastrophic thinking, fear of activities associated with the persons condition and perceived levels of disability. The research project aimed to provide an evaluation of the PGAP on two levels. How effective is the program at reducing the four psychosocial risk factors associated with work related disability and does participating in the PGAP improve the persons readiness to return to work?
To answer these questions, we contacted 29 people who had been referred to Adaptive Workplace Solutions as a result of a work-related injury or condition. Of those contacted 20 provided consent to participate in the research and their results from the PGAP were gathered to analyse the effectiveness of the program. Each persons’ file was reviewed, and they were allocated a work readiness score at referral and upon completion of the program.
The results of the research project demonstrated that the PGAP was effective in reducing the identified psychosocial risk factors associated with prolonged absence from the workforce and increased work disability. This result was consistent with the international research on the PGAP. The other aim of the study was to assess the improvement’s in work readiness following participation in the PGAP. The data indicated that 75% of people who had participated in the PGAP had an improvement in return to work readiness. The other interesting finding was that people who experienced improvements in two or more of the psychosocial risk factors were more likely to also experience improved return to work readiness scores. In summary, the results support the inclusion of the PGAP in work injury rehabilitation where people are at risk of experiencing psychosocial risk factors associated with return to work.
In the Position Statement ‘What is Good Work?’ (2013) written by the Australasian Faculty of Occupational and Environmental Medicine (AFOEM*) of The Royal Australasian College of Physicians (RACP), it is stressed that not all work has a beneficial impact on health. They detail 5 key domains of good work, but also highlight individual differences and the importance of a good fit between the individual and the work tasks and environment. What is beneficial for one person may be harmful for another. In order to reap the health, social and economic benefits of work, it is essential for governments, regulators, insurers, business leaders and employers to focus on what constitutes “good work” while also ensuring a good match between the individual and the role.
According to AFOEM’s ‘Consensus Statement on the Health Benefits of Good Work’ (2017), good work:
• is engaging, fair and respectful
• balances job demands, autonomy and job security
• accepts the importance of culture and traditional beliefs
• is characterised by safe and healthy work practices
• strikes a balance between the interests of individuals, employers and society
• requires effective change management and clear and realistic performance indicators
• matches the work to the individual
• uses transparent productivity metrics.
Under this definition of good work, they acknowledge the following principles:
• The provision of good work is a key determinant of the health and wellbeing of employees, their families and broader society.
• Long term work absence, work disability and unemployment may have a negative impact on health and wellbeing.
• All workplaces should strive to be both healthy and safe.
• Providing access to good work is an effective means of reducing poverty and social exclusion.
• With active assistance, many of those who have the potential to work, but are not currently working, can be enabled to access the benefits of good work.
• Safe and healthy work practices, understanding and accommodating cultural and social beliefs, a healthy workplace culture, effective and equitable injury management programs and positive relationships within workplaces are key determinants of individual health, wellbeing, engagement and productivity.
• Good outcomes are more likely when individuals understand, and are supported to access the benefits of good work especially when entering the workforce for the first time, seeking re-employment or recovering at work following a period of injury or illness.
For more detail and information please refer to the following references.
References:
Royal Australasian College of Physicians (RACP) Website – Health Benefits of Good Work
‘Realising the Health Benefits of Good Work Consensus Statement’ (2017) Australasian Faculty of Occupational and Environmental Medicine (AFOEM)
‘What is Good Work?’ (2013) Australasian Faculty of Occupational and Environmental Medicine
Return to Work SA Health Benefits of Work Fact Sheet

Article Review by Kelly Alderson
The Vocational Rehabilitation Index (VRI) is a tool which can measure personal factors in return to work after a compensable injury. In this research, data was collected from 461 participants in NSW who had a Whole Person Impairment over 10%.
The VRI considers
| Personal | Most Risk | Lower Risk |
| Age^ | 41 – 50 years old | 31 – 40 (16 – 30 close to this) |
| Gender^ | Male | Female |
| Occupation | Unskilled (low skilled roles) | Professionals |
| Length of time away from work^ | Over 2 years | 13 – 24 months |
| Spinal Injury*1 | Disc injury (lower back) | Whiplash |
| Psychological Condition*2 | Minor and Major conditions | No psychological condition |
| Labour Market* 3 |
*1 Spinal Injuries – there was no evidence that the seriousness of spinal injury is a predictor.
*2 Psychological conditions – these were broken into major and minor. Across both of these domains, the people presenting with these conditions were approximately 3 times less likely to return to work. What is not clear in this article is if there is any difference between those with a primary or secondary claim and the absence or presence of a psychological condition that is not compensable. However, I think we could draw some inferences about this. Interestingly, this did not meet the threshold for statistical significance. It may be that if these items were teased out further, that there may be an effect that would meet the requirements for statistical significance.
*3 Labour Market – We contacted the author about this and he did clarify this point. He advised that less than ¼ of participants had returned to work. He further explained that the data was drawn from areas of high unemployment and so the labour market did not seem to have an effect, but he did note that this created some bias in the data.
^ denotes that the finding met the threshold for statistical significance.
The above table provides a profile for risk which can be helpful for determining whom might be suitable to refer for vocational rehabilitation services, although there are probably other triggers that should be considered also. For example; perceived injustice, poor relationship with the pre-injury employer and failure to engage with a return to work plan.
In regards to time away from work, it is interesting that this research suggests that the best return to work rates came out of the 13 – 24-month cohort. Although, it is important to note that this data is related to those with a whole person impairment over 10%. In regard to risk, those with an injury around the 12 month mark were also at higher risk and therefore need careful consideration.
We asked the author a couple of questions about the research, in particular if they thought that there is a link between occupation (unskilled or low skill) and readily transferable skills. Dr Athanasou agreed with this observation and added that this is also reflective of the data set and it being drawn from areas with higher levels socioeconomic and sociocultural disadvantage. So it is possible that other confounding variables may be at play as well, in terms of what we know about socioeconomic disadvantage. For example, poorer health outcomes (ABS, 2018a) because people in this group tend to access less preventative health services, they are at high risk of social exclusion, have more difficulty affording noncompulsory education, in fact year 12 completion rates have increased nationally, but there is no evidence that those residing in high levels of socioeconomic disadvantaged have followed this trend (ABS, 2018a). It is a hypothesis of mine, that part of the picture in terms of return to work, is that a work injury is likely to have a larger impact on this group because of pre-existing disadvantages and this is likely to deepen should redeployment be required. This adds an additional layer of complexity to an already complex picture.
With this in mind, we then need to look forward to solutions. Truth be told, there are a bunch of solutions that are well outside of the scope of Return to Work, for example improving base level language and literacy skills. Although this is important, it is not always going to be achievable, but there are some other considerations. For example, in terms of suitable duties plans, are we wasting a potential opportunity here? Don’t get me wrong, I am not suggesting that we ‘throw the baby out with the bath water’ and stop them as they are critical for other reasons. But there is more need now than ever before to make sure that these are targeted and timely because wasting 6 months in a work placement that is not going to lead to employment and is not serving the worker any skill development opportunities, is potentially wasting valuable time. Sure, if you are 100% confident that the person will get back to pre injury duties, it is probably fine. However, if you are sitting on the fence in terms of a goal, then based on this article, the best bang for your buck in terms of a placement is developing potential employability skills that are currently missing or underdeveloped (this may require some vocational counselling to workout an alternative goal and what needs to be achieved skill wise). This way, best case scenario the person returns to work and they have learnt some new skills, but worse case scenario, the goal needs to be reviewed and the person has already tried out another role and has already started accumulating the skills required to be successful in securing employment (plus they have a reference who will be able to hopefully help them secure that next job (if it does not arise out the placement).
So the next issue is how can we get employers to engage in mentorships for their staff or those needing a placement. But I think that this is a topic for another day.
If there are other topics you would like us to review or review, please comment below and we will add this to our list.
Reference:
ABS . (2018a, March). http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4250.0.55.001Main Features32009.
ABS. (2018b, March). http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by Subject/1370.0~2010~Chapter~Socioeconomic disadvantage (4.1.7.4).
Athanasou, J. (2018). A Vocational Rehabilitation Index and Return to Work after Return to Work after Compensable Occupational Injuries in Australia. The Australian Journal of Rehabilitation Counselling, 69-78.

