Adaptive Workplace Solutions can now offer Psychology Services!


Kelly and Kate have both achieved their Provisional Psychologist Registration, meaning they can now both offer:
- Psychological Treatment Services
- Psychological Worksite Assessments
- Vocational Assessments
This is an exciting new phase for Adaptive Workplace Solutions as we broaden our service provision to ensure the most effective services are available to both our clients and our referrers.
Congratulations to both Kelly and Kate – what wonderful achievements!!

What do I need to know about sleep?
Sleep is a natural process that allows the brain and body to rest and recover. When you are asleep, your eyes are closed, most of your muscles are relaxed, and your consciousness is practically suspended. But while your body is still, your brain is quite active.
Sleep is important as it helps us restore and recover ourselves physically while also assisting us to organise things in our brain. People need sleep in order to function well – mentally and physically.
Going without sleep or having insufficient sleep can lead to a range of issues including:
• Poor mood / feelings of depression
• Lack of concentration
• Irritability
• Low motivation
• Heart disease
• Blood pressure
• Diabetes
• Increased likelihood of road accidents or workplace accidents
Sleep can be affected by a range of things including ageing, lifestyle commitments, injury, trauma, stressors, health problems, anxiety, depression, medication.
However a regular sleep pattern CAN be re-established after a disruption, even a significant disruption.
Sleep cycle
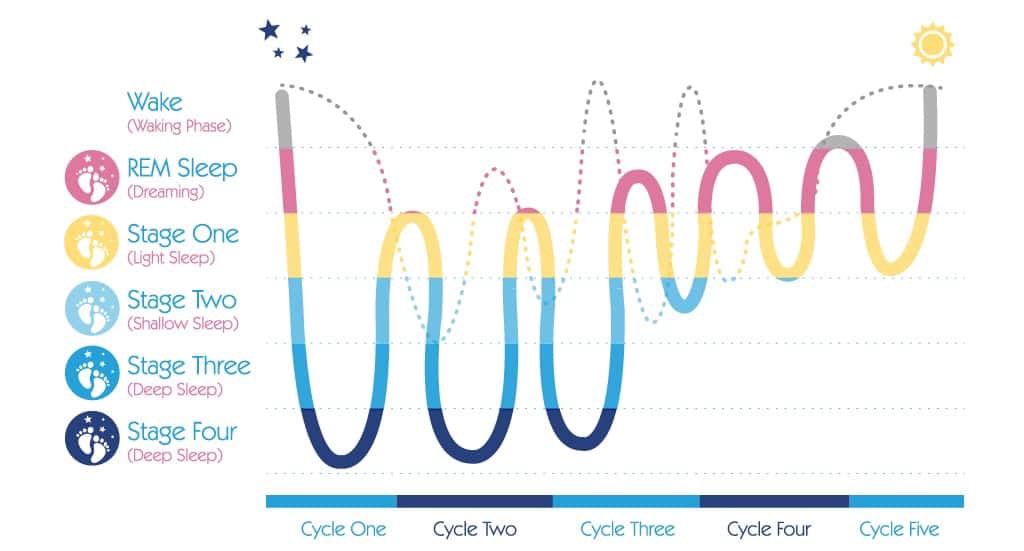
Sleep occurs in cycles that last around 90 minutes per cycle. During each cycle, different types of brain activity occur.
5 stages of sleep have been identified based on this brainwave activity:
Stage 1: Drowsiness. This is often referred to as the transition between awake and asleep. The eyes are generally closed, but the person awakens easily. If disrupted during this period, people will often state that they were not yet asleep or were just resting. This usually lasts for around 5-10 minutes
Stage 2: Light sleep. This sleep stage involves spontaneous periods of muscle activity mixed with periods of muscle relaxation. The heart rate slows and body temperature decreases. The body prepares to enter deep sleep.
Stages 3 and 4: Deep Sleep. Also known as slow-wave or delta sleep. During these stages the breathing is more relaxed, heart rate slows, sound and light sensitivity diminish. It is difficult to wake someone while in a deep sleep. Quality sleep needs to include deep sleep. Often when people seem to have had sufficient sleep (as measured by hours of sleep) but are still tired and fatigued each morning, it may be that they are not achieving deep sleep in their cycle. This deep sleep is vital in the secretion of the growth hormone. This hormone is necessary to restore the body and if this does not occur, people can be more prone to infections and disease. Alcohol, medication and stress can all impact on your ability to achieve deep sleep.
Stage 5: REM (Rapid Eye Movement) sleep. Also known as dream sleep. During REM sleep there is heightened brain activity, but the mind paralyses the muscles, possibly to keep the body from acting out the dreams and harming itself. The first period of REM typically lasts around 1 minutes, with each recurring REM stage becoming longer. The final stage may last around an hour. REM sleep is vital for normalising cognitive and emotional activities.
How much sleep do we need?
Different people require different amounts of sleep, which changes over a person’s life span. The average for an adult is around 7-8 hours, but anything within 5–10 hours can be normal.
The best guide to whether you are having enough sleep is how you function throughout the day. If you are sleepy and struggle to concentrate it is likely you are not getting enough sleep.
The first 3-5 hours of sleep is when the deepest sleep occurs (see graph above). This is the most restorative.
Waking up a few times during the night is quite normal and nothing to be concerned about. This usually occurs during the periods of light or REM sleep spaced out over the night. Being concerned or worried about waking up generally increases the likelihood of it being difficult to get back to sleep and increase these awake periods.
Sleep deprivation Scale
The Epworth Sleepiness Scale (ESS) can provide a measure of the impact of sleep deprivation on daytime function. This should only be used by people not on sleep medication.
If you feel you may be deprived of sleep and are not taking any sleep medication, completing this quick scale can give you an indication of how much impact it is having on your life:
0 would never doze
1 slight chance of dozing
2 moderate chance of dozing
3 high chance of dozing
Situation Rating
Sitting and reading ______
Watching TV ______
Sitting inactive in a public place (e.g. movie or meeting) ______
Passenger in a car for 1 hour with no break ______
Lying down in the afternoon when circumstances permit ______
Sitting and talking to someone ______
Sitting quietly after a lunch without alcohol ______
In a car, while stopped for a few minutes in traffic ______
TOTAL ______
Score indicator:
0-4 Satisfactory daytime functioning
5-9 Daytime tiredness, lack of energy
>10 Excessive daytime sleepiness
Sleep Diary
If you feel you have an issue with sleep or score 5 or above on the Epworth scale, the first step in making change can be to record relevant information in a sleep diary for 4-5 days in a row. This should give a clear indication of a baseline pattern and can identify potential problem areas and solutions.
Each day record:
• any daytime naps and their duration
• number of cups of tea, coffee, cola or energy drinks and approx. time each one was consumed
• number of standard drinks of alcohol and approx. time of consumption
• any sleep medication and time taken
• time when you go to bed
• approx. time when you fall asleep
• number of times you wake through the night and approx. indication of how long you were awake for
• time when you wake
• time when you got out of bed
It is important not to be too obsessed with clock watching or it will interfere with your natural pattern. This is particularly the case when waking in the night – clock watching will only increase the time you are awake for. An estimate of your sleep behaviours is fine.
Creating Positive Change
People who are having difficulties with sleep during the night often try to go to bed earlier or stay in bed longer to “catch up” on their sleep. This generally makes the problem worse, as more time is spent lying in bed awake. Often people feel anxious or frustrated about not sleeping during this time, which can build up an association between being in bed and negative emotions.
It is not necessarily easy to re-set your sleep pattern. It needs commitment and persistence. Initially you are likely to feel tired and irritable and may even get less sleep as your body adjusts to a new pattern. You will often feel more tired during the day, but it is important not to nap until the pattern is established.
Be aware it may take from 4-6 weeks to notice any improvement – repetition and consistency is key.
Effective Strategies:
• The most effective strategy when re-introducing a sleep pattern is ensuring a regular wake-up time. Stick to this wake-up time 7 days per week, even if you feel you haven’t had much sleep during the night.
• Get sunlight within 10-15 minutes of waking if possible.
• Only go to bed when you feel sleepy rather than at a fixed time in the evening.
• Establish a regular evening sleep routine – this is a pattern of behaviour that tells your body and mind it is time to go to sleep.
• Only stay in bed if you are sleeping. If you are lying in bed awake for more than 20 minutes, get up and do something relaxing in another room until you feel tired again.
• Only use the bed/bedroom for sleep or sexual intimacy. Avoid laying in the bed to rest during the day or using the bedroom to watch TV, eat, smoke, work, play computer games or chat on your phone.
• Avoid taking daytime naps.
During the Day:
• Keep a regular routine for meals, medication and general daily activities
• Pace your activities throughout your day
• Spend time outdoors in the afternoon if possible
• Avoid napping
• Keep as active as possible
• Reduce coffee to no more than 3 cups per day
During the evening:
• Relax and prepare for sleep
• Utilise an hour of quiet activity before you intend to sleep
• List what is on your mind and organise to do it tomorrow (to avoid worrying or planning throughout the night)
• Learn and use a relaxation tool to switch off. This may be a breathing exercise, mindfulness, meditation, or something that works for you.
• Avoid exercise late in the evening – light exercises early in the evening can be helpful
• Avoid caffeine for at least 5 hours before bedtime
• Avoid smoking before bedtime and during wakening
• Avoid alcohol near bedtime
• Avoid a heavy meal too close to bedtime
• Reduce disturbing noises and be calm about the unavoidable
• Avoid screentime – particularly laptops and mobile phones for one hour before bed
At bedtime:
• Develop a bedtime routine and follow it every night
• Recognise any emotional responses for what they are and use appropriate coping techniques to deal with such responses
• Only go to bed when you feel ‘sleepy tired’, not when you are just physically exhausted or you think its time for bed
• Keep reading and TV for another room
• Avoid using your bed for anything other than sleep or sexual intimacy
• Do not lie in bed awake for longer than 15-20 minutes
• During that 15-20 minutes enjoy relaxing in bed if you do not fall straight to sleep
• Use relaxation techniques to induce sleep
• Prepare somewhere to go (e.g. another room) and something to do if you do have to get up
• Return to bed only when you feel sleepy again
• Repeat the rising routine as frequently as necessary
• Keep the bedroom dark
When getting up in the morning:
• Get up at the same time each morning
• Have a routine that refreshes and takes your needs into account
• Allow time to avoid demanding morning routines
• Make a plan for the day
• Ensure that you have at least one rewarding activity.
Important tips when trying these strategies:
• Rather than being discouraged if there are lots of things you have identified that you can change, be pleased that you have identified a number of things that can help as this increases your chance for improvement.
• Don’t expect to have great results overnight – improvement may take 4-6 weeks.
• Change can take longer if the reasons for the sleep disruption are more complex. Be patient with yourself and take things one step at a time.
• It can be helpful in the initial stages to focus on behaviours/strategies you can ADD rather than things you need to avoid or stop doing.
• Feeling tired throughout this process of change is totally normal – feeling sleepy during the day is often one of the last things to disappear.
• A habit is learned and established by consistent repetition over long periods of time – it might be hard, but don’t give up!
SUMMARY: Tips to Sleep Better
• Stick to a consistent wake up time – even on the weekends. This helps to regulate your body’s clock and could help you fall asleep and stay asleep for the night.
• Practice a relaxing bedtime ritual. A relaxing routine activity right before bedtime conducted away from bright lights helps separate your sleep time from activities that can cause excitement, stress or anxiety.
• Avoid daytime naps – particularly in the afternoon. Power napping may help you get through the day, but if you find that you can’t fall asleep at bedtime, eliminating even short catnaps may help.
• Exercise daily. Vigorous exercise is best, but even light exercise is better than no activity. Exercise at any time of day, but it is best to avoid vigorous exercise for a few hours before bedtime.
• Avoid alcohol, caffeine, cigarettes and heavy meals in the evening. You may feel that alcohol or heavy meals make you tired enough to fall asleep, but these can interrupt with the natural sleep cycle and may lead to waking early or not getting sufficient deep sleep.
• Wind down – Your body needs time to shift into sleep mode, so spend the last hour before bed doing a calming activity such as reading, talking, or listening to music. For some people using an electronic device such as a laptop or phone can make I hard to fall asleep because the particular type of light coming from the screens is activating to the brain. If there are any activities that you associate with anxiety about sleeping, remove them from your bedtime routine.
• Evaluate your room. Design your sleep environment to establish the conditions you need for sleep. Your bedroom should be on the cooler side (around 15-19 degrees). It should also be free from any noise and light that can disturb your sleep. If you have environmental distractions you can’t remove, try using eye shades, ear plugs, white noise machines, or other devices.
• Sleep on a comfortable mattress and pillows – Make sure your mattress and pillow is comfortable and supportive.
• If you can’t sleep, don’t just lay there – go into another room and do something relaxing until you feel tired.
• Use your bed only for sleep and sex to strengthen the association between bed and sleep.
Our Rehabilitation Counsellors can help you to implement these strategies and improve your sleep health. Contact us today for more information if you need additional assistance.

In order to combat unhelpful thinking styles you must learn to leave your negative thoughts behind. The trick is not just to stop the ongoing storm of thoughts, but rather to change the nature of the thoughts from destructive to positive and life-enhancing ones.
As you commit yourself to eliminating these negative ways of thinking, you must understand two factors. First, these unhelpful thinking patterns are much more likely to emerge when you are fatigued or highly stressed,or when there is a significant problem facing you. These situations weaken your ability to cope and contribute to distorted thinking. Ironically, these bad thinking habits emerge when there’s a problem, and that’s exactly when effective coping responses are needed most. When things are going reasonably well, they may not be apparent at all.
Also, many people do not experience these thought disorders with all problems. These habits instead tend to emerge when a problem touches on an area of personal vulnerability or emotional sensitivity. By noticing exactly when distorted patterns emerge, you can pinpoint unresolved personal conflicts, thereby enhancing your personal awareness. These emotional “soft spots” clearly call for strengthened coping skills.
How do you get rid of these self-defeating ways of thinking?
It can be done, but will require self-awareness, patience, practice and support.
Here are some helpful hints:
- Verbalise your thoughts when a problem occurs.
To build awareness of distorted thinking, think out loud when you have a problem. You may even need to record yourself and play it back. If you have a trusted friend you could run your thoughts past them to see how they sound when said aloud to another person. You may be very surprised at how negative and self-defeating your thoughts actually are. Remember that these thoughts reinforce negative perceptions of you and reality.
- Do not project thoughts onto other people.
It’s easy to attribute unfairly negative thoughts to loved ones or close friends. To eliminate distorted thinking, first take full responsibility for your thoughts. Then open yourself to give other people a chance to care about you.
- Work on one habit at a time.
Most people are prone to several different negative thought patterns. To tackle them all at once is usually self-defeating. Instead, identify one distorted thinking habit and work on that one alone until it is eliminated. Then move onto another one until you overcome all of them.
- Act as if you are completely competent and in control (Fake it until you make it!)
In the beginning, force yourself to do this in lieu of negative thinking in order to give new ways of relating to a problem a chance. You will feel better because problems don’t seem so overwhelming, and you are coping more effectively. “What you say to yourself, you become.”
- Use thought-stopping as a technique.
When you find yourself slipping into distorted thinking, internally shout to yourself, “STOP!”
STOP -> THINK –> Then TALK/ACT
- Practice positive affirmations.
Even when you feel good, it’s helpful to make self-reinforcing statements. However, these need to be realistic and practical. Saying “everything will be wonderful in the end” may not be helpful, because sometimes things do not turn out this way. However, saying “No matter what obstacles are thrown at me, I am strong enough to overcome them” is quite different. Whether you initially believe it or not, practising saying it aloud will reinforce those beliefs and you will start to believe them. No matter where you are, keep your self-affirming thoughts going.
- Put positive suggestions by others into practice.
It is often helpful to ask for and really listen to feedback from your partner or a good friend. When you do, make it a point not become defensive, because receiving feedback often triggers negative thinking. You may find yourself gaining insight into how to cope more effectively.
- Separate yourself from negatively thinking peers.
Often negative perceptions are reinforced by friends, especially when discussing personal or relationship struggles. If you need to talk it out, find one upbeat friend who is helpful to use as a sounding board.
Bottom line: It’s very difficult, if not impossible, to live life happily when you feel insecure, unloved, distrustful of others, and threatened by events around you. But most of these feelings you create yourself. You can’t change the world, but you can change yourself and the way you perceive life events.


You don’t need special skills to support someone in need. Asking, “Are you OK?” with kindness, concern and in a genuine way can make a world of difference. A day to help to inspire and empower everyone to meaningfully connect with people around them and support anyone struggling with life.
In 1995, much-loved Barry Larkin was far from ok. His suicide left family and friends in deep grief and with endless questions.
In 2009, his son Gavin Larkin chose to champion just one question to honour his father and to try and protect other families from the pain his endured.
“Are you OK?”
The extraordinary story behind R U OK? was brought to life by Australian Story in 2011.
We know that suicide prevention is an enormously complex and sensitive challenge the world over. But we also know that some of the world’s smartest people have been working tirelessly and developed credible theories that suggest there’s power in that simplest of questions – “Are you ok?”
One of the most significant theories is by United States academic, Dr Thomas Joiner. 1 Because his father took his own life, Thomas has dedicated his research to try and answer that question “why?”
His theory tries to answer that complex question by describing three forces at play in someone at risk. The first force is the person thinks they’re a burden on others; the second is that they can withstand a high degree of pain; and the third is they don’t feel connected to others.
It’s this lack of connection (or lack of belonging) that we want to prevent. By inspiring people to take the time to ask “Are you ok?” and listen, we can help people struggling with life feel connected long before they even think about suicide. It all comes down to regular, face-to-face, meaningful conversations about life. And asking “Are you ok?” is a great place to start.
As well as helping you start these conversations, we’re working with experts in the field to monitor how these conversations impact on Australia’s suicide rate.
HOW TO ASK:
By starting a conversation and commenting on the changes you’ve noticed, you could help that family member, friend or workmate open up. If they say they are not ok, you can follow our conversation steps to show them they’re supported and help them find strategies to better manage the load. If they are ok, that person will know you’re someone who cares enough to ask.
For more information or to Donate to support such a meaningful fund please visit:
Counselling (24/7)
If you need further support please contact one of the following numbers
• Lifeline Australia – 13 11 14
• Lifeline New Zealand – 0800 543 354
• Kids Helpline – 1800 55 1800
• MensLine Australia – 1300 78 99 78
• Suicide Call Back Service – 1300 659 467
• Beyond Blue – 1300 22 4636
• Veterans and Veterans’ Families Counselling Service – 1800 011 046

The Progressive Goal Attainment Program (PGAP®) is an evidence-based treatment program targeting psychosocial barriers to recovery and rehabilitation for clients suffering from debilitating health or mental health conditions. It is a highly researched standardized intervention for reducing disability associated with a wide range of debilitating health and mental health conditions. The PGAP is supported by empirical data and has been demonstrated to reduce disability and contribute to successful return-to-work in individuals with conditions including back pain, whiplash, fibromyalgia, cancer, depression, and PTSD.
The primary goal of the PGAP is to reduce psychosocial barriers to rehabilitation progress. This goal is achieved through the use of evidence-based techniques specifically designed to target psychosocial risk factors.
The PGAP includes:
• Cognitive-behavioural techniques such as thought-monitoring and reappraisal;
• Behavioural techniques such as graded exposure and goal setting;
• Relational techniques such as disclosure and validation.
The PGAP would be considered a CBT intervention, with a primary focus on behaviour change. CBT techniques have been adapted such that ‘disability reduction’ is the central objective of treatment as opposed to symptom management.
Finally, the evidence base speaks clearly in favour of the PGAP, particularly as it pertains to return-to-work outcomes. In all clinical trials of the PGAP, return to work has been the primary outcome variable. A list of scientific publications supporting the use of the PGAP as a return-to-work intervention can be accessed through the www.PGAPworks.com website.
Within our team, both Kelly Alderson and Cass Hill are trained and experienced in the provision of the Progressive Goal Attainment Program. We have found it to be of extreme benefit to the majority of clients who have engaged in the program. For more information on how the PGAP can assist you or your clients or to find out more information regarding this service, please feel free to contact us for further discussion.
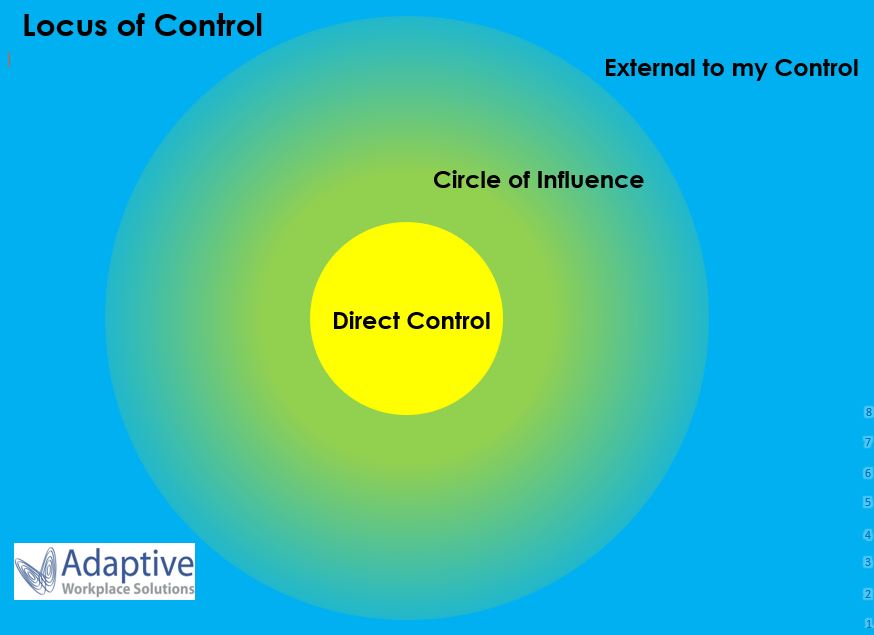
Locus of Control is the extent to which people believe they have power over their lives. This concept was developed by Julian Rotter in the 1950s and is widely accepted within psychology today. We have observed that many of our clients who have difficulties with successfully returning to work after an injury have an external locus of control, in other words they believe that outside forces are directing their personal outcomes. They often focus excessively on worries or concerns that are external to their control and don’t tend to take responsibility for their own successes or failures. Most of their energy is spent in the blue section of the image above. This can serve as a barrier to their progress and return to work goals. As a comparison, people who have an internal locus of control believe that they can influence events and take responsibility for their own actions and outcomes. They invest their energy in the yellow section of the image above, focusing on what they can either directly control or have some level of influence over.
If you are noticing a worker who blames others for their lack of progress, puts events down to fate or luck, expresses that other people (e.g. their doctor, employer) are in control of their situation or doesn’t take responsibility for their own actions (positive or negative) it might be that they need some assistance before they are able to move forward. Heightening their awareness of the parts of their life that they can influence is a key aspect of assisting with this. Opening up a conversation about what aspects of their current situation they feel are realistically outside of their control and then discussing the things that they can affect or impact is a great starting point. Positive goal setting can also be helpful as it draws attention to direct action they can take. If you have tried those steps and are finding your client is stuck in unhelpful thinking patterns, it may be that we can help! Adaptive Workplace Solutions have developed a tool shown in the image above which we have used with many clients with great results. When used along with counselling and home activities, we have had an excellent success rate of assisting clients to shift their locus of control, enabling them to gain a healthy level of control over their lives. Many clients have named it as pivotal in changing their perspective and allowing them to take steps towards returning to work.