We would like to welcome our two students from Flinders University, Far and Candice to our Adaptive Workplace Solutions team for the next few months while they complete their final placements with us. They are both in their fourth and final year of a Bachelor in Disability and Developmental Education with a major in Rehabilitation Counselling. They will be shadowing our staff members to learn as much as they can about the role, while also engaging in their own projects throughout their placements. They will both be involved in as many different aspects of the role as they can, including meetings with clients, Return to Work Specialists / Case Managers, employers, medical treatment providers and case conferences, so please make them feel very welcome!

My name is Far Boonkun and I’m currently in my last year of my Bachelor of Disability and Developmental Education with a major in Rehabilitation Counselling. I have been on placement with Adaptive Workplace Solutions for several weeks now, shadowing various staff members to learn and absorb anything and everything about rehabilitation services for the Return to Work SA system.
I am passionate about helping people and providing support for people and people with disabilities in whatever area they need and require. I am currently juggling support work and bartending but when I am not working or studying, I enjoy going to live gigs, stand up and drag shows, reading and I try to travel when I can! Although I just spent 5 months in North America and went to Thailand in April.
I am looking forward to learning the ins and outs of this area and am very excited to graduate this year!

Hi, My name is Candice and I am a 4th year student at Flinders University studying Disability and Developmental Education with a major in Rehabilitation Counselling. I have been fortunate enough to be offered a final placement at Adaptive Workplace Solutions initially starting out one day a week but soon extending to full time hours until the end of November.
During my time on placement I will be working on a couple of projects one of them being developing some easy-read resources to sit alongside the Progressive Goal Attainment Program Workbook and also developing some further resources for pain education.
My background is in disability services and I am passionate about supporting people with disability achieve their full potential. When I am not at work or studying I enjoy spending time at the gym, cooking, gardening and going out to dinner with my partner.
Wednesday the 24th of July is Stress Down Day. Here are our tips for reducing stress!
#1 Identify symptoms and causes of stress
In order to reduce stress, we first must be aware of the symptoms of stress and also identify the causes. Signs of stress vary from person to person, but may include tensing your jaw, grinding your teeth, difficulty sleeping, muscle tension, headaches, feeling irritable or short tempered, lack of concentration or motivation, feeling overwhelmed, depressed or anxious, and overuse of alcohol or drugs as a coping mechanism. Sometimes it can be difficult to identify the cause of stress and there are often multiple factors involved, so keeping a journal to track your stressors may be useful. Clearly identifying what is causing the stress is the first step in doing something about it. Sometimes the cause of stress can be eliminated, and at other times it is about developing more effective coping mechanisms.
#2 Use problem-solving to eliminate the cause of stress
Once you have determined the cause of stress, some stressful situations can be eliminated, reduced or changed by problem solving. It is often helpful to write down a list of possible solutions, work through the pros and cons of each, select the best one, try it out and evaluate its success. Focus on the things that are within your control. If you have multiple stressors it is generally best to focus on one at a time.
#3 Organise and manage your time effectively
Research suggests that good time management can decrease stress, increase satisfaction with work and life and generally improve health. Some strategies to improve your time management include setting goals, prioritising tasks, using a diary or to-do lists to track tasks and progress and delegating work to others. It is important to accept that not everything can be done at once and list tasks according to genuine priority. Being organised can also be as simple as sorting out your morning routine to avoid rushing or tidying up your work area for a calmer and more productive work day.
#4 Practise relaxation techniques
Practising relaxation techniques regularly has been found to reduce stress. This can include a range of activities such as: meditation, breathing exercises, progressive muscle relaxation or mindfulness. These techniques can help reduce stress levels by allowing the body and nervous system to settle into a calm state. They don’t need to take long, just one minute of focus on breathing or mindful noticing of the tangible things you can experience with your 5 senses can help if practised regularly. Different methods will be effective for different people – you might have to try a few approaches before you find something that works for you. There are lots of apps available that can help you add some relaxation techniques to your busy lifestyle. Structured activities such as Yoga, Pilates can be beneficial too!
#5 Look after your health
Stress can affect your immune system and make you more vulnerable to a range of health conditions. Keeping yourself fit and healthy can improve your resilience and enable you to cope more effectively with stressful situations.
🥗 Eat a healthy and well balanced diet
🥛 Drink plenty of water
🚫 Avoid or reduce consumption of alcohol, caffeine, nicotine and other drugs, especially if you are overusing these to cope
❌ Avoid or reduce intake of refined sugars as they can cause energy crashes and lead you to feel tired and irritable
🏌️♀️Ensure you get some physical activity each day and exercise regularly

#6 Increase Daily Physical Activity
Stressful situations increase the level of stress hormones such as adrenaline and cortisol in your body. These are the “fight or flight” hormones designed to protect us from bodily harm when we are under threat. However it is unlikely that your stressful situation will require a physical fight or flight response and so physical exercise can be used to metabolize the excess stress hormones and restore your body to a calm and relaxed state. 🧘🏾♀️
Additionally, regular physical exercise is good for your general health and well-being and can keep you feeling positive and more able to cope with stressful situations when they arise. Simple changes to your daily routine such as going for a 30 minute walk during your lunch break or kicking the footy with your kids after work can make a BIG difference!!
#7 Ensure you are getting enough sleep
A lack of sleep is a significant cause of stress, however it can also be a symptom of stress as thoughts whirling around your head can make it difficult to fall asleep. If sleep is an issue for you, it can help to create a relaxing evening routine that gets you prepared and ready for sleep and aim to go to bed at the same time each night so your mind and body can get into a good sleep pattern. Avoid caffeine and excessive alcohol in the evenings as these can lead to disturbed sleep patterns. Don’t engage in mentally engaging activities for a few hours before bedtime to allow your brain time to calm down. Turning off screens (TV, smartphones, laptops) at least one hour before bed can also help. Some helpful activities to do before bedtime include some light reading, talking quietly with the lights dimmed, or taking a warm shower or bath.
#8 Rest if you are unwell
Often we can be guilty of putting too much pressure on ourselves, and contributing to our own stress. A good example of this is feeling like we have to carry on, even when we are unwell. A short rest can often help the body to recharge and recover from illness. Whether this means taking a day off work when you are sick, or simply letting some of your other responsibilities (such as housework) go for a short time while you recover. Looking after yourself is very important!!
#9 Learn to say no
A common cause of stress is having too much to do and too little time to complete it. And yet, in this predicament so many of us still agree to take on additional responsibility when asked. Learning to say “no” to additional or unimportant requests can assist in reducing stress and may even lead to an increase in confidence and self-esteem.
To learn to say “no” requires an understanding of why you find it difficult. Many people find it hard to say “no” because they want to help and are trying to be nice and be liked. For others it can be a fear of rejection or missed opportunities. Understanding what drives you can assist you in taking control and ensuring that you are placing as much importance on your own time and health as you do for others.
#10 Make time for things you enjoy
Take your mind off your worries by ensuring you allow plenty of time for enjoyable activities. This may feel impossible if you are overwhelmed with too much to do, however taking a bit of time out for yourself to do something positive or fun may ultimately lead to better coping skills and increased productivity. Ideas may include gardening, listening to music, socialising, going to the gym, getting into nature, reading, taking a bubble bath… the list is endless! What is your favourite enjoyable activity that you find helps to alleviate stress?

#11 Create a healthy work-life balance
Work plays a very big role in our lives, but it’s important to balance this with other life activities. If work is increasing your stress levels, think about other areas of your life that you would like to focus on (eg. Relationships, exercise, recreation, social activities) and how you can also prioritise these aspects in your daily life.
Taking time to wind down and enjoy relaxing activities is an important part of balanced life and helps to reduce stress. Include relaxing as well as uplifting activities into your daily or weekly routine.
#12 Stay away from conflict. Resolve issues when they arise.
Interpersonal conflict takes a toll on our physical and emotional health. Its a good idea to avoid conflict at work and in your personal life as much as possible. Surround yourself with positive people that make you feel good about yourself as much as you can. Avoid gossip or discussing volatile topics (such as religion or politics) at work. If conflict finds you anyway, learn positive ways to deal with it and ask for support if you need to.
#13 Resist perfectionism
Mistakes shouldn’t be feared – they are an opportunity to learn and improve! The desire to be perfect can make your stress spike and your self-worth plummet. Recognise that you are not defined by your failures, instead see them as an opportunity for improvement and self-discovery. Remember no one is perfect – and people who may appear that way on the outside may be struggling with their own unrealistic perfectionistic standards.
#14 Practise positive self-talk
When we are stressed we often say negative or self-defeating things to ourselves over and over. Unhelpful self-talk may include things like “I can’t cope”, “I’m too busy to deal with all of this”, “I’ll never get this done” or even “I’m completely useless”. Notice this self talk and think about more constructive ways to talk to yourself. Practise saying positive statements to yourself, ensuring they are realistic and that you believe them. Suggestions could be “I am coping well given what I have on my plate at the moment”, or “This is tough at the moment but I know I’ll get through it and things will be easier on the other side”.
Try and keep things in perspective – when we are stressed it is easy to catastrophise and see things as far worse than they really are. Ask yourself “how likely is it that that negative event will happen?” or “am I overestimating how bad the consequences will be?”
#15 Talk to someone
Its okay to need support sometimes. Don’t be afraid to admit when you need help to enable you to cope. There are a range of people you can talk to when you are feeling stressed, for example, family members, co-workers, supervisors, bosses, doctors or psychologists. Your employer may have stress management resources available or your doctor may be able to refer you to a psychologist or mental health professional. If you are feeling overwhelmed it is a good idea to ask for support, especially if it is prolonged over a period of time.

At Adaptive Workplace Solutions we frequently organise work placements for clients as part of their return to work and rehabilitation plan. Work placements are vital for injured workers who are unable to return to their place of employment to re-establish positive work habits, gradually increase their duties and develop new skills.
Why someone may need a work placement
Generally after a work injury, the injured worker returns to their place of employment quickly on a graduated return to work plan starting with light duties. However, in some cases, there are no light duties available (due to the size of the employer, the nature of the work etc) and a person may need a suitable work placement for a short period of time in order to build up their capacity and strength before returning to their pre-injury role.
In other cases, a person’s specific injury may prevent them returning to either their workplace or their role in which case they would be working towards a new employment goal. This pathway may include some training and will almost always include some on the job experience, building vital skills through a voluntary work placement.
Benefits to the Worker
- Retain or Regain positive work habits. If people are out of work for a prolonged period it can be hard to get back into a good routine for work. It is better for people to keep up their routine through attending a workplace regularly rather than have an extended period off work and then try and rebuild these habits.
- Social component of work. It can be very isolating for people to be off work through a work injury. Work provides valuable opportunity for socialising and being part of a community.
- Mental Health. Purposeful and valued activity at work promotes positive mental health.
- Physical conditioning. Attending work is an important part of people’s physical recovery. A work placement provides an opportunity for a graduated plan, where tasks and time at work can be increased gradually, allowing the person to regain their strength, stamina and ability to engage in everyday work-related tasks. It is important that all medical restrictions are taken into consideration and that the person only engages in duties within their capabilities, allowing them to build up steadily.
- Skill Building. When a goal of new employment is set, a work placement provides a great opportunity to build skills for the new role and develop confidence.
- Experience and Pathway to New Employment. When applying for new employment, most employers look for people with experience. A work placement provides an opportunity to gain experience in a new role, and potentially even a glowing reference. This will put them in good stead when applying for new jobs.
Benefits to the Host Employer
- Additional team member at no extra cost. Who couldn’t benefit from a free extra set of hands during busy times? A work placement is completely unpaid, so the host employer benefits from the extra staff member and all of the experience, knowledge and skills they bring for the duration they are there.
- Insurance is covered. We understand that many potential employers have concerns about the implications for their business if the person was to make their injury worse, or re-injure themselves while on placement. Return to Work SA cover the insurance for all of these potential situations, as well as any damage that the worker on placement may accidentally cause. This gives peace of mind that there is no risk to taking someone on for a work placement.
- Promoting a diverse workplace. Having someone on work placement can add to the diversity of your workplace culture.
- Contributing to the community. It can give business owners and host employers a great feeling to know that they have helped someone to get back on their feet by assisting them with important steps in their rehabilitation.
- Incentives to offer paid employment. Sometimes host employers are so impressed with the person there on placement that they want to offer them a paid position. This is not an expectation during a work placement, but it is a great bonus for all parties if it is the right fit. In this case the placement provides an opportunity to test out an employee to see if they are a good fit before offering employment. Return to Work SA provide the RISE scheme, a financial incentive for employers to take someone on after a work injury.
How does it work?
Generally, we will contact relevant workplaces to arrange a work placement that is a good fit for that individual client and their needs. At that point, when a host employer expresses interest, we set up a meeting involving the host employer, the client and an Adaptive Workplace Solutions staff member. This meeting gives the host employer the chance to meet with the client and see if they will be a good fit. We can also discuss practical considerations including time component, any medical restrictions that need to be followed etc. From there a placement agreement is drawn up and signed by all parties and the person can begin!
We frequently require host employers across the whole Adelaide and Hills area to support clients with work placements in a range of industries. If you think that your workplace may be interested in taking someone on for a work placement or have light work duties frequently available, we would love to hear from you. Give us a call today and we can discuss how you can get involved!

Today we welcome Nicola Marsh, Physiotherapist to our team!

Nicola brings a wealth of physiotherapy clinical experience to her role at Adaptive Workplace Solutions. She is experienced in:
- Clinical assessments
- Management and treatment of a range of musculoskeletal injuries and conditions
- Setting up of gym programs and home exercise programs
- Pain neuroscience education
- Teaching of active coping skills such as progressive muscle relaxation and mindfulness
- Short and long term goal setting
- Increasing meaningful activity involvement through pacing plans
- Teaching strategies to overcome flare ups
Nicola is passionate about assisting clients to achieve their goals in order to return to work and valued activities outside of work. This is done through high quality assessments, evidence based recommendations and guiding clients towards the use of self-management strategies.
We are very excited to have Nicola join our team and are looking forward to her valuable input!

In order to combat unhelpful thinking styles you must learn to leave your negative thoughts behind. The trick is not just to stop the ongoing storm of thoughts, but rather to change the nature of the thoughts from destructive to positive and life-enhancing ones.
As you commit yourself to eliminating these negative ways of thinking, you must understand two factors. First, these unhelpful thinking patterns are much more likely to emerge when you are fatigued or highly stressed,or when there is a significant problem facing you. These situations weaken your ability to cope and contribute to distorted thinking. Ironically, these bad thinking habits emerge when there’s a problem, and that’s exactly when effective coping responses are needed most. When things are going reasonably well, they may not be apparent at all.
Also, many people do not experience these thought disorders with all problems. These habits instead tend to emerge when a problem touches on an area of personal vulnerability or emotional sensitivity. By noticing exactly when distorted patterns emerge, you can pinpoint unresolved personal conflicts, thereby enhancing your personal awareness. These emotional “soft spots” clearly call for strengthened coping skills.
How do you get rid of these self-defeating ways of thinking?
It can be done, but will require self-awareness, patience, practice and support.
Here are some helpful hints:
- Verbalise your thoughts when a problem occurs.
To build awareness of distorted thinking, think out loud when you have a problem. You may even need to record yourself and play it back. If you have a trusted friend you could run your thoughts past them to see how they sound when said aloud to another person. You may be very surprised at how negative and self-defeating your thoughts actually are. Remember that these thoughts reinforce negative perceptions of you and reality.
- Do not project thoughts onto other people.
It’s easy to attribute unfairly negative thoughts to loved ones or close friends. To eliminate distorted thinking, first take full responsibility for your thoughts. Then open yourself to give other people a chance to care about you.
- Work on one habit at a time.
Most people are prone to several different negative thought patterns. To tackle them all at once is usually self-defeating. Instead, identify one distorted thinking habit and work on that one alone until it is eliminated. Then move onto another one until you overcome all of them.
- Act as if you are completely competent and in control (Fake it until you make it!)
In the beginning, force yourself to do this in lieu of negative thinking in order to give new ways of relating to a problem a chance. You will feel better because problems don’t seem so overwhelming, and you are coping more effectively. “What you say to yourself, you become.”
- Use thought-stopping as a technique.
When you find yourself slipping into distorted thinking, internally shout to yourself, “STOP!”
STOP -> THINK –> Then TALK/ACT
- Practice positive affirmations.
Even when you feel good, it’s helpful to make self-reinforcing statements. However, these need to be realistic and practical. Saying “everything will be wonderful in the end” may not be helpful, because sometimes things do not turn out this way. However, saying “No matter what obstacles are thrown at me, I am strong enough to overcome them” is quite different. Whether you initially believe it or not, practising saying it aloud will reinforce those beliefs and you will start to believe them. No matter where you are, keep your self-affirming thoughts going.
- Put positive suggestions by others into practice.
It is often helpful to ask for and really listen to feedback from your partner or a good friend. When you do, make it a point not become defensive, because receiving feedback often triggers negative thinking. You may find yourself gaining insight into how to cope more effectively.
- Separate yourself from negatively thinking peers.
Often negative perceptions are reinforced by friends, especially when discussing personal or relationship struggles. If you need to talk it out, find one upbeat friend who is helpful to use as a sounding board.
Bottom line: It’s very difficult, if not impossible, to live life happily when you feel insecure, unloved, distrustful of others, and threatened by events around you. But most of these feelings you create yourself. You can’t change the world, but you can change yourself and the way you perceive life events.

Mary – PROGRESSIVE GOAL ATTAINMENT PROGRAM (PGAP)
When we started working with Mary, she was a 36-year-old married lady with three school-aged children. She had been involved in a work accident 10 months prior and had suffered an injury to her shoulder. She had maintained contact with her employer during that time but had not made any attempt to return to work. She presented with significant symptoms of depression, was often teary and struggled to get through her daily responsibilities with her family.
When we met, Mary’s main reported issues were her high levels of pain and her overall feeling of being completely overwhelmed by everything she needed to fit into her week. Initial discussions regarding a return to work sent Mary into quite a panicked state, and she struggled to even discuss or contemplate this. Although she was not at work, she was participating in a range of treatments for her shoulder including physiotherapy 3 times per week, massage once a week and GP visits once a fortnight. Mary was extremely stressed about how she could fit all these appointments in as well as care for her family. She no longer felt that she was in control of her own life. She reported that her personal and social life had suffered – she was not meeting with friends, spending time with her husband and felt that she was no longer an active participant in her children’s lives. Mary explained that her behaviour had changed significantly, and reported herself as being far more snappy and critical than usual.
Mary’s initial assessment measures indicated severe reported pain levels, moderate depressive symptoms, severe symptoms of post-traumatic stress and severe levels of fatigue. Her psychosocial measures demonstrated high levels of catastrophic thinking and perceived injustice and moderate levels of perceived disability.
Throughout the 10 week program, we focused on:
- A daily walking program;
- Increasing meaningful activity involvement;
- Planning and scheduling daily activities;
- Focusing on one day at a time so as to not become overwhelmed;
- Goal setting;
- Breaking goals down into achievable parts;
- Addressing and challenging thought patterns relating to her perceived injustice and catastrophic thinking.
Initially, we assisted Mary to focus on the things that were most important to her – her children, husband, extended family and friends. We also did some goal-setting around taking time out for herself. Setting some goals around these crucial elements of her life and then scheduling time to actively engage in meaningful and enjoyable activities gave her a very quick sense of success, achievement and she reported starting to feel some control over her life. The daily walking program assisted in re-establishing a ‘normal’ morning routine where she would get up earlier, shower, get dressed and have breakfast before leaving the house for a walk. She also included her family inthis walk whenever possible, which became an enjoyable time to spend some time together outdoors and discuss their plans for the day which also providing some exercise and fresh air.
By week 4, Mary was ready to start a graduated return to work program, starting on light duties and with reduced hours. Organising a case conference with Mary, her doctor and her physiotherapist really reinforced the importance of giving work a try and gave Mary the confidence she needed to know that everyone was assisting her and monitoring her progress and that if something went wrong she had people to assist her get back on track.
By the end of the 10 week program, Mary was successfully maintaining 3 days per week at 5 hours per shift. She was meeting with friends once per week and had broadened her friendship circle though her school network. She reported feeling more confident as a mother and felt that she had gained important parenting strategies along the way that assisted her to cope. Her assessment measures also noted significant progress with only mild reported pain levels (even though her activity levels had significantly increased), sub-clinical symptoms of depression, mild symptoms of post-traumatic stress and moderate levels of fatigue. Her perception of disability had reduced to low and her perceptions of injustice and catastrophic thinking patterns had reduced to moderate (see graph). Mary had enjoyed the daily planning structure so much that she had made this into an ongoing routine, even on completion of the program. At the end of the program we revised tools and strategies for coping and getting back on track if things started getting difficult again.
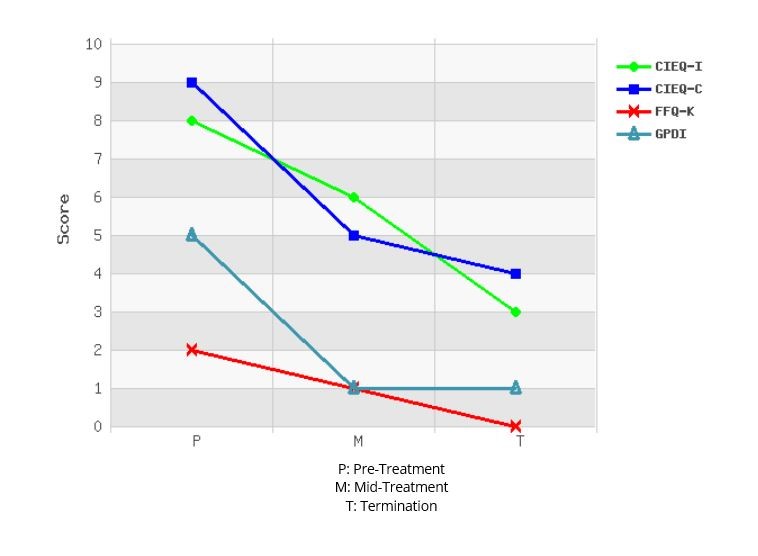
Six months on, and Mary has continued and maintained her journey of progress. She is maintaining her pre-injury work hours (4 full days per week) and reports thatshe is enjoying work again. She has continued to use her daily planning structure to not overwhelm herself with planned activities and ensure that she makes time for herself, her family and some social outings. Although she still feels some discomfort in her shoulder at times, and feels that she gets tired more easily than she used to, she is not reporting any pain.
Mary’s case
study demonstrates the importance of:
- Focusing on the whole person, including what is happening physically,cognitively, socially, emotionally, relationship-wise and work-wise;
- Involving other key treatment providers in the program so everyone is working towards the same goals;
- Starting goal setting with meaningful life goals if the return to work goals are too overwhelming at that stage;
- Using the success of the life/social goals and activity scheduling towork towards the return to work goals;
- Using very gradual increments and pacing to break large goals down into smaller achievable ones.


You don’t need special skills to support someone in need. Asking, “Are you OK?” with kindness, concern and in a genuine way can make a world of difference. A day to help to inspire and empower everyone to meaningfully connect with people around them and support anyone struggling with life.
In 1995, much-loved Barry Larkin was far from ok. His suicide left family and friends in deep grief and with endless questions.
In 2009, his son Gavin Larkin chose to champion just one question to honour his father and to try and protect other families from the pain his endured.
“Are you OK?”
The extraordinary story behind R U OK? was brought to life by Australian Story in 2011.
We know that suicide prevention is an enormously complex and sensitive challenge the world over. But we also know that some of the world’s smartest people have been working tirelessly and developed credible theories that suggest there’s power in that simplest of questions – “Are you ok?”
One of the most significant theories is by United States academic, Dr Thomas Joiner. 1 Because his father took his own life, Thomas has dedicated his research to try and answer that question “why?”
His theory tries to answer that complex question by describing three forces at play in someone at risk. The first force is the person thinks they’re a burden on others; the second is that they can withstand a high degree of pain; and the third is they don’t feel connected to others.
It’s this lack of connection (or lack of belonging) that we want to prevent. By inspiring people to take the time to ask “Are you ok?” and listen, we can help people struggling with life feel connected long before they even think about suicide. It all comes down to regular, face-to-face, meaningful conversations about life. And asking “Are you ok?” is a great place to start.
As well as helping you start these conversations, we’re working with experts in the field to monitor how these conversations impact on Australia’s suicide rate.
HOW TO ASK:
By starting a conversation and commenting on the changes you’ve noticed, you could help that family member, friend or workmate open up. If they say they are not ok, you can follow our conversation steps to show them they’re supported and help them find strategies to better manage the load. If they are ok, that person will know you’re someone who cares enough to ask.
For more information or to Donate to support such a meaningful fund please visit:
Counselling (24/7)
If you need further support please contact one of the following numbers
• Lifeline Australia – 13 11 14
• Lifeline New Zealand – 0800 543 354
• Kids Helpline – 1800 55 1800
• MensLine Australia – 1300 78 99 78
• Suicide Call Back Service – 1300 659 467
• Beyond Blue – 1300 22 4636
• Veterans and Veterans’ Families Counselling Service – 1800 011 046
Beliefs and Definitions of pain
Historically, humans have been very interested in the pain experience and have had a wide variety of explanations regarding pain.
In Ancient Greece 500 BC they believed that pain occurred when the Goddess of revenge, “Poine” was sent to punish fools who had angered the gods. Treating pain involved prayer and animal sacrifice.

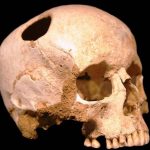
Many ancient cultures believed that pain was something inside the person which had become stuck and needed removal.
Holes were drilled into body parts and sometimes pipes were used to “suck the pain out”.

During the 1600s there were giant leaps in scientific understanding.
Rene Descartes proposed the idea that pain was a mechanical sensation transmitted to the brain. The body part that had been injured sent a message up to the brain where it could be received and understood as pain. In order to treat the pain either the injured body part needed to be fixed or the message needed to be stopped.
We have largely held onto this understanding of pain into current times. We only need to watch advertisements for commonly used painkillers to see images involving pain being transmitted from the injury to the brain and then the painkiller smashing away the transmission to stop the message before getting to the brain. Research has clearly shown that pain is far more complicated than this, through studies of people with phantom limb pain after amputation and a variety of other examples that clearly demonstrate that pain actually does not correlate well with degree of injury.
So what then is pain? There have been many attempts at defining pain.
Some of the more useful ones include:
“Pain is whatever the person in pain says it is.” – McCafferey (a nurse) 1968
“Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” – The International Association for the Study of Pain (1994) and the World Health Organisation (2007)
“Pain is a construction in the brain to help us deal with threat, either real or perceived via a change in behaviour.” – Mature organism Model, Gifford (1998)
“Pain is a multiple system output activated by an individual specific pain neurosignature; the neurosignature is activated whenever the brain concludes that the body tissues are in danger and action is required.” – Lorimer Moseley (2003)
These more recent explanations of pain focus on threat and danger; pain is explained as a mechanism produced by the brain to protect us from harm. Physical harm (e.g. accidentally putting your hand onto the hotplate) is reasonably easy to understand. The combination of nociception (the activation of physical receptors to physical changes such as pressure, temperature and chemical change) as well as the visual perception of danger causes the brain to produce a pain response. This causes the physical response of quickly moving your hand away from the hotplate and perhaps running it under cold water. The pain response is not only caused by the physical stimulus of heat, but also by our awareness that leaving our hand on the hotplate could potentially lead to a severe burn (that is, our perception that the situation is potentially dangerous).
However, pain can occur in a variety of situations where there is no physical damage.
One example of this was documented in the British Medical journal in 1995. A builder jumped down onto a nail in a building site, which went right through his foot and was sticking out through the top of his shoe. Understandably, the man was screaming in considerable pain. He would not allow anyone to remove his shoe as the slightest movement caused extreme pain. He required sedation and strong pain medication to enable him to be x-rayed (with the shoe still on), to discover that the nail had actually gone straight between his toes and had not penetrated his foot at all – not even a scratch!

It may be easy to think that this pain is somehow not “real” as there was no damage. However, his pain is equally as real as if the nail had indeed gone right through his foot. In this case the visual perception, combined with previous experience involving serious injuries on the worksite was enough to cause the brain to decide the situation was extremely dangerous and that pain was required to ensure the danger could be resolved.
In other examples, people have had horrendous injuries and not experienced much, if any pain.
In 2010 Jonathan Metz had been trapped in his basement for approximately three days with his arm stuck in the furnace and little chance of being found chose to saw off his own arm in order to escape, and survive. After the traumatic incident explained his surprise at not experiencing much, if any pain through the process. He certainly expected it to hurt and felt physically sick looking at what he was doing, however only mild pain was felt. This can easily be explained through this threat model of pain, as his brain had come to the conclusion that the threat of being locked in the basement was far more dangerous than the threat of cutting off his arm. In the absence of a perception of danger involved, no pain needed to be produced. There are many similar examples in the area of sport, where athletes feel little or no pain during or immediately after a severe physical injury.
Important things we now know about pain
- No scan or test can tell if someone is feeling pain or not. X-rays, CT scans and MRI results have been consistently demonstrated to be very poorly correlated with the experience of pain.
- No one else can feel your pain
- ALL pain is real
- You cannot imagine pain
- Pain can be weird (e.g. delayed pain, phantom limb pain, pain that spreads to unrelated areas)
- Nociceptive nerve fibres are triggered by chemical change (e.g. inflammation), physical events (e.g. pressure), and temperature changes
- Nociceptive nerve fibres can adapt and amplify their signals through frequent triggering, generally leading to increased pain with reduced activity levels
- Pain is influenced (positively and negatively) by mood, concerns, thoughts, perception of control, importance placed on the injury, and a range of other cognitions.
- Pain can be influenced by boom/bust behaviour and flare ups
So what does this all mean?
Pain is useful and should not be ignored. Pain is a protective mechanism generated by the brain in response to perceived threat. However, when pain is persistent and there is no direct or immediate threat to the body, understanding how the body can get “stuck” in pain can suggest ways to help it get “unstuck.”
All current evidence leads to the conclusion that PAIN IS CHANGEABLE!
Pain is produced by the brain and we also know that the brain is constantly going through changes. Neuroplasticity can be defined as the brain’s ability to reorganise itself by forming new neural connections throughout life. Neuroplasticity allows the neurons (nerve cells) in the brain to compensate for injury and disease and to adjust their activities in response to new situations or to changes in their environment. Examples of this include learning a new skill, developing a taste for certain types of food and recovering from stroke. Dr Norman Doidge, A psychiatrist and researcher from the University of Toronto in Canada has highlighted the importance of neuroplasticity for healing a range of conditions from long term pain to Parkinson’s disease in his bestseller The Brain That Changes Itself (2007).
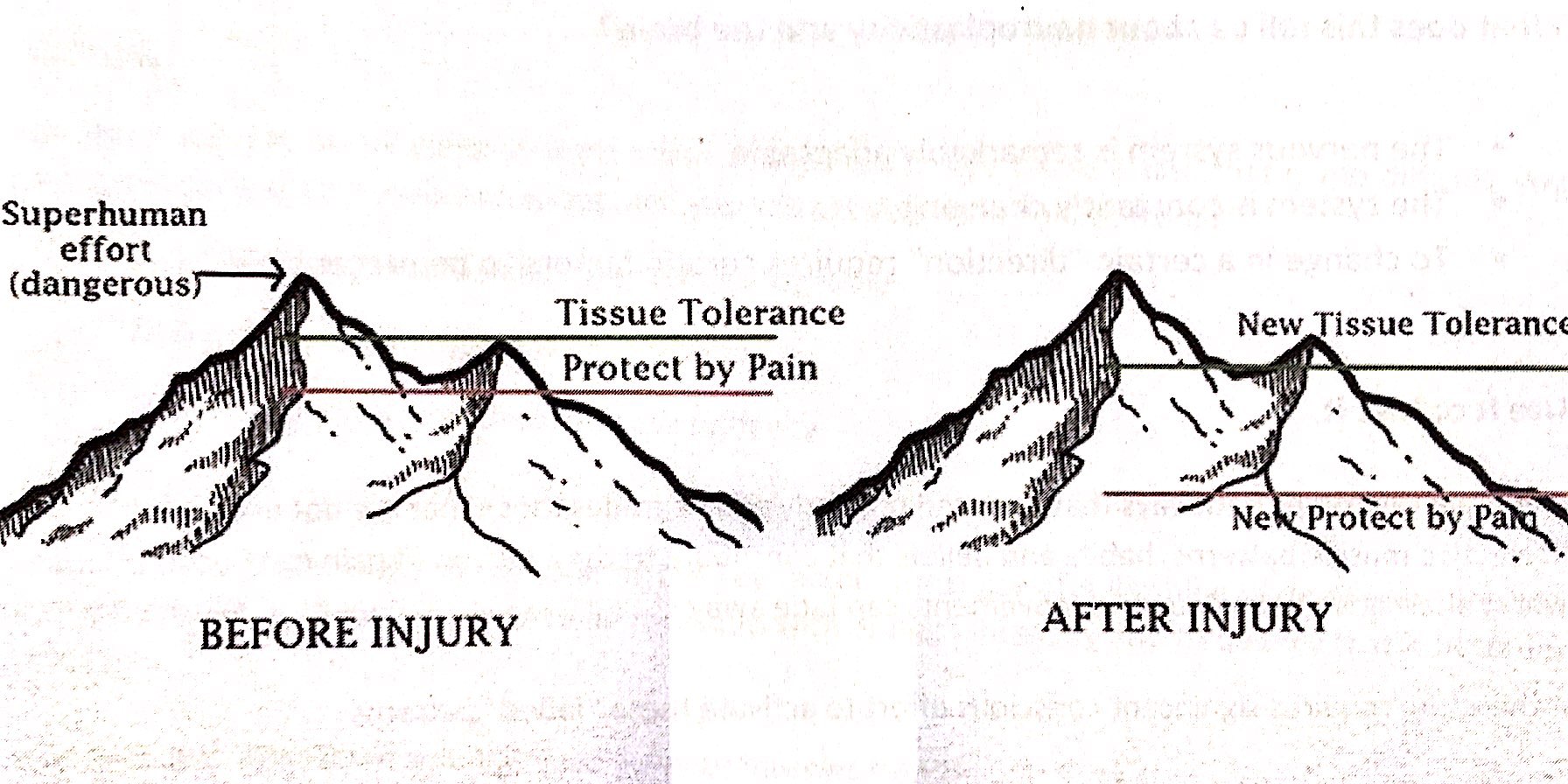
Everyone has a tissue tolerance level, that is a threshold where activities go from being safe to being dangerous. This differs between individuals and can also change over time through inactivity, exercise, strength training etc. When pain is working effectively, the protect by pain line sits under the tissue tolerance level so that as we begin to approach our tissue tolerance threshold, pain kicks in to remind us to stop or slow down or at least let us know we are reaching our limits. After an injury, the tissue tolerance level may slightly reduce as newly healed structures may not be quite as strong or capable as before. Most healing will be complete after 6 weeks (often much sooner, depending on the injury) meaning it is safe to go back to physical activity. However, in persistent pain problems, the protect by pain level has significantly dropped, so that even the slightest activity can be enough to set off the pain signal.
The key point to focus on is that these changes have primarily happened within the brain and the brain can be retrained. This retraining allows the protect by pain line to slowly and steadily increase until it is once again sitting just under the new tissue tolerance line. This is done through pain education and gradual exposure to safe activities through a pacing program. It is important that people know that even though it may hurt, the activity is safe. Building up slowly increases confidence and decreases the fear and threat of danger. The new tissue tolerance line can also be changed through safe exercise and strengthening activities. People do not have to suffer ongoing pain indefinitely.
At Adaptive Workplace Solutions we can provide pain education combined with meaningful goal setting and pacing/graded exposure plans to assist people with ongoing pain problems get back to everyday activities for work, play and life! If you would like further information please contact us to talk to one of our consultants in more detail. For further reading, we highly recommend the book Explain Pain by Dr David Butler and Dr Lorimer Moseley.
In the Position Statement ‘What is Good Work?’ (2013) written by the Australasian Faculty of Occupational and Environmental Medicine (AFOEM*) of The Royal Australasian College of Physicians (RACP), it is stressed that not all work has a beneficial impact on health. They detail 5 key domains of good work, but also highlight individual differences and the importance of a good fit between the individual and the work tasks and environment. What is beneficial for one person may be harmful for another. In order to reap the health, social and economic benefits of work, it is essential for governments, regulators, insurers, business leaders and employers to focus on what constitutes “good work” while also ensuring a good match between the individual and the role.
According to AFOEM’s ‘Consensus Statement on the Health Benefits of Good Work’ (2017), good work:
• is engaging, fair and respectful
• balances job demands, autonomy and job security
• accepts the importance of culture and traditional beliefs
• is characterised by safe and healthy work practices
• strikes a balance between the interests of individuals, employers and society
• requires effective change management and clear and realistic performance indicators
• matches the work to the individual
• uses transparent productivity metrics.
Under this definition of good work, they acknowledge the following principles:
• The provision of good work is a key determinant of the health and wellbeing of employees, their families and broader society.
• Long term work absence, work disability and unemployment may have a negative impact on health and wellbeing.
• All workplaces should strive to be both healthy and safe.
• Providing access to good work is an effective means of reducing poverty and social exclusion.
• With active assistance, many of those who have the potential to work, but are not currently working, can be enabled to access the benefits of good work.
• Safe and healthy work practices, understanding and accommodating cultural and social beliefs, a healthy workplace culture, effective and equitable injury management programs and positive relationships within workplaces are key determinants of individual health, wellbeing, engagement and productivity.
• Good outcomes are more likely when individuals understand, and are supported to access the benefits of good work especially when entering the workforce for the first time, seeking re-employment or recovering at work following a period of injury or illness.
For more detail and information please refer to the following references.
References:
Royal Australasian College of Physicians (RACP) Website – Health Benefits of Good Work
‘Realising the Health Benefits of Good Work Consensus Statement’ (2017) Australasian Faculty of Occupational and Environmental Medicine (AFOEM)
‘What is Good Work?’ (2013) Australasian Faculty of Occupational and Environmental Medicine
Return to Work SA Health Benefits of Work Fact Sheet

The Progressive Goal Attainment Program (PGAP®) is an evidence-based treatment program targeting psychosocial barriers to recovery and rehabilitation for clients suffering from debilitating health or mental health conditions. It is a highly researched standardized intervention for reducing disability associated with a wide range of debilitating health and mental health conditions. The PGAP is supported by empirical data and has been demonstrated to reduce disability and contribute to successful return-to-work in individuals with conditions including back pain, whiplash, fibromyalgia, cancer, depression, and PTSD.
The primary goal of the PGAP is to reduce psychosocial barriers to rehabilitation progress. This goal is achieved through the use of evidence-based techniques specifically designed to target psychosocial risk factors.
The PGAP includes:
• Cognitive-behavioural techniques such as thought-monitoring and reappraisal;
• Behavioural techniques such as graded exposure and goal setting;
• Relational techniques such as disclosure and validation.
The PGAP would be considered a CBT intervention, with a primary focus on behaviour change. CBT techniques have been adapted such that ‘disability reduction’ is the central objective of treatment as opposed to symptom management.
Finally, the evidence base speaks clearly in favour of the PGAP, particularly as it pertains to return-to-work outcomes. In all clinical trials of the PGAP, return to work has been the primary outcome variable. A list of scientific publications supporting the use of the PGAP as a return-to-work intervention can be accessed through the www.PGAPworks.com website.
Within our team, both Kelly Alderson and Cass Hill are trained and experienced in the provision of the Progressive Goal Attainment Program. We have found it to be of extreme benefit to the majority of clients who have engaged in the program. For more information on how the PGAP can assist you or your clients or to find out more information regarding this service, please feel free to contact us for further discussion.

